With maternal deaths highest among Black women, some are shunning traditional care during their pregnancies.
Midwife Victoria Buchanan hears a common refrain from pregnant Black women in her care:
“Oh, I just don’t want to die,” Buchanan said they tell her. “I just want to come out of here alive. I want to have a healthy baby. I want to be next to my kids.”
Buchanan, 28, believes that she and the team at Sentara Midwifery Specialists in Hampton, Va., can keep new mothers and their babies healthy and defy the bleak statistics linked to Black pregnancies. Research shows that Black women in the United States are three times more likely to suffer a pregnancy-related death than white women. In Virginia, Black women in recent years have been more than twice as likely as other mothers to have a death attributed to childbirth.

As a nonprofit journalism organization, we depend on your support to fund journalism that addresses the crisis of institutionalized racism in America. Donate any amount today to become a Pulitzer Center Champion and receive exclusive benefits!
The national crisis for Black maternal health came into even sharper focus recently with a pair of high-profile cases. Tori Bowie, a world-champion sprinter and Olympic gold medalist, died in May from childbirth complications. Bowie, eight months pregnant and in labor at the time of her death, was found lifeless in her home, alone. She was 32.
And tennis legend Serena Williams has shared how she struggled to get medical professionals to take her seriously when she suffered serious health complications after giving birth.
Both cases highlight the risks that Black women — even those with celebrity, accomplishment and wealth — face during childbirth. And study after study back up their stories.
Health experts say the country should be doing much more to improve maternal health and reach levels equal to other developed nations. More than 8 in 10 pregnancy-related deaths in the United States could have been prevented, according to research by the Centers for Disease Control and Prevention.
The Practice

Midwife Marsha Jackson holds 6-week-old Rose Poosz — daughter of Raynesha Sharpe — during a well-baby check at BirthCare & Women’s Health in Alexandria, Virginia. Jackson plans to retire at the end of this year. She estimates she’s delivered nearly 4,000 babies without losing a mother in childbirth. Her success rate counters a stark national statistic: Black women in the United States are three times more likely to suffer a pregnancy-related death than white women. Image by Karen Kasmauski. United States.
Aiming to improve the health of expectant Black mothers, public health officials and providers have been looking at the role midwives can play — particularly as research has shown that the use of skilled midwives may prevent a significant number of maternal deaths.
In building a 2021 strategic plan to address Virginia’s disparities in maternal health, the administration of then-Gov. Ralph Northam met with health care officials and professionals across the state — including midwives and doulas — and recommended increasing the use and support of midwifery. In certain instances, Medicaid in Virginia covers midwifery costs. Private health insurance varies in its coverage of midwife services.
Advocates say they have seen how the holistic approach taken by midwives — listening to prospective parents, educating them, coordinating health care and performing home births — is linked to better health outcomes for women of color. And when midwives are of the same race as their patients, some say there is a level of reassurance that comes from knowing their caretaker understands their situation and will be an advocate for them.
Photographer Karen Kasmauski followed the work of Black midwives between January and April this year in Virginia. Her series of photographs traces the relationships formed between midwives and their clients — from initial consultations and prenatal meetings to the birth and support in the months following pregnancy.

Nichole Wardlaw, a former teacher who has been a midwife for almost two decades, serves military and civilian families in Hampton Roads. She said she feels the maternal health system remains biased and too often ignores the pain and symptoms of distress that women of color have during pregnancy.
“I get a lot of clients, especially Black women, who have had trauma during their last pregnancies,” Wardlaw said. “They didn't like how they were treated at the hospital. They did not appreciate not feeling heard or supported. That seems to be a recurring theme.”
Marsha Jackson, a midwife in Alexandria, Va., who co-founded BirthCare & Women’s Health in 1987, sees a steady demand for her services.
“I think one of the main reasons women seek out midwives is because they want that personalized care,” Jackson said. “They want someone to take time and to listen.”
Jackson and the midwives in her practice typically spend more time with pregnant women than the patient would get at a standard practice, she said.
Clients also have more input into their care with a midwife. “We work together,” Jackson said. “It’s a shared responsibility.”
— Interviews by Karen Kasmauski

Using props and a small doll, Ebony Simpson, a midwife at BirthCare & Women’s Health in Alexandria, Virginia, demonstrates to Raynesha Sharpe how the baby enters the birth canal. Seated beside Sharpe is her 14-month-old child, Romeo Poosz, who was born in a hospital due to his mother’s stalled labor. Image by Karen Kasmauski. United States.

The midwives at BirthCare & Women’s Health work on submitting required paperwork for re-accreditation by the Commission for the Accreditation of Birth Centers. CABC accredits developing and existing birth and midwifery centers in the U.S. It was the Saturday before the documents were due and an all-hands-on-deck situation — though some of the midwives would have to break away from the task to deliver babies in the second-floor birthing rooms. Even though it is a small business, the Alexandria, Virginia, center must meet the same requirements as large hospitals that are equipped with administrative staff. Pictured from left: midwives Dorothy Lee; Marsha Jackson, seated; Martha Weaver; and Ebony Simpson and office assistant Amauri Holton, who is also in training to become a birth assistant. Image by Karen Kasmauski. United States.

At her business BirthCare & Women’s Health in Alexandria, Virginia, co-founder Marsha Jackson displays photographs of babies she has delivered since 1981, when her career as a midwife began. Image by Karen Kasmauski. United States.
In Virginia, the maternal mortality rate for White, non-hispanic women in 2019 was 44.9 pregnancy-associated deaths per 100,000 births, the rate for Black women that year was 103.3.
source: the Virginia Department of Health’s Virginia Maternal Mortality Review Team Triennial Report: 2018-2020

Midwife Ebony Simpson demonstrates how to turn a baby that is facing the wrong direction during an educational meeting for birth assistants at BirthCare & Women’s Health in Alexandria, Virginia. Several birth assistants — who work with midwives as independent contractors during the birthing process — are also training to be midwives. Image by Karen Kasmauski. United States.

Midwives Ebony Simpson, far left, and Marsha Jackson, back to camera, lead a tour of BirthCare & Women’s Health in Alexandria, Virginia, for a group from Durham, North Carolina — from center left, Amber Rodriguez, midwife Tina Braimah and financial adviser Heather Wilson. The three, who are looking to start their own birthing center, said they see a great need for midwives in their community, especially among underserved mothers. Image by Karen Kasmauski. United States.
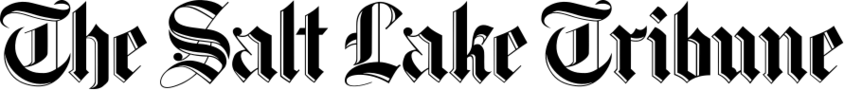
Amoni Thompson-Jones and her husband, Casey Jones, meet with midwife Ebony Simpson at BirthCare & Women’s Health in Alexandria, Virginia. After Thompson-Jones took her own blood pressure, which all the women do before their appointments, Simpson determined it was high enough to run an EKG on the pregnant woman. Here, Simpson goes over the results with Jones while Thompson-Jones — who was within weeks of her due date — rests behind them. Image by Karen Kasmauski. United States.

Amoni Thompson-Jones holds the hand of her husband, Casey Jones, during a contraction in their Alexandria, Virginia, apartment. Midwife Ebony Simpson was called to the home for the birth, but the labor stalled. After a lack of progression, and with Thompson-Jones showing signs of distress, midwife Marsha Jackson was called in around 3 a.m. Because Thompson-Jones’ blood pressure was high, Jackson made the decision to take her to a nearby hospital in Alexandria, where she eventually had a cesarean section. Image by Karen Kasmauski. United States.
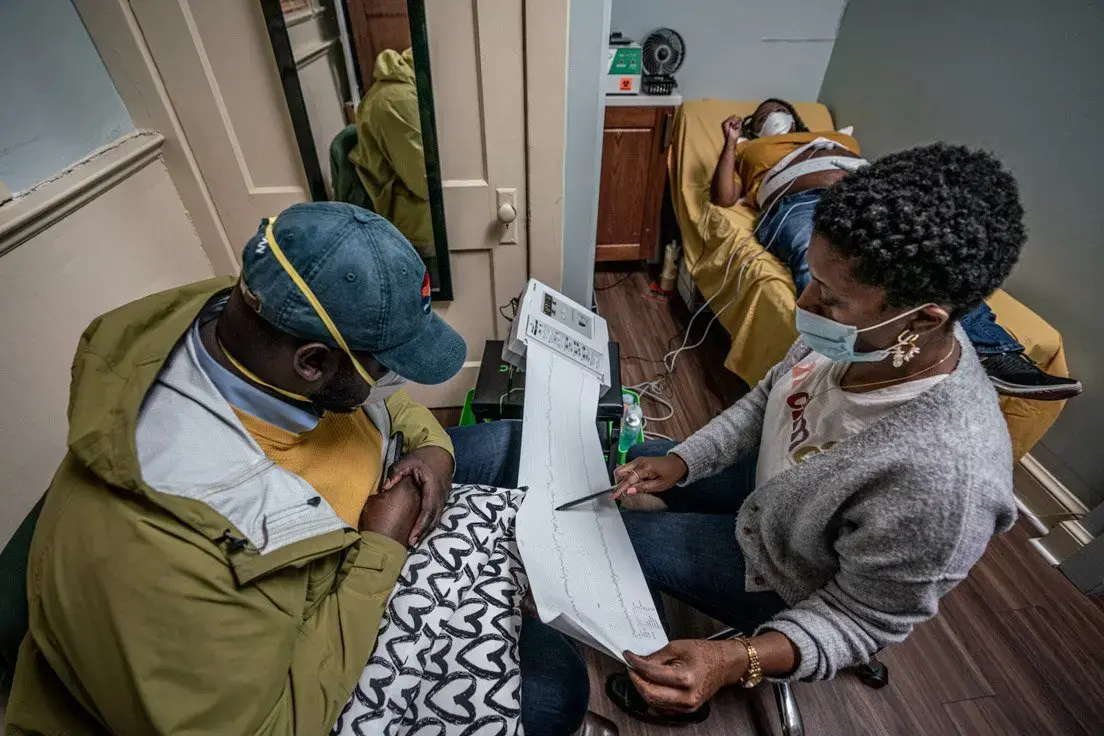
Midwife Marsha Jackson gets information on how to complete the recertification process for BirthCare & Women’s Health in Alexandria, Virginia. The center must be recertified every three years. Image by Karen Kasmauski. United States.

Lit by the afternoon sun coming in through the window blinds, Amara Thompson rests in her father’s hands in their apartment in Alexandria, Virginia. Image by Karen Kasmauski. United States.
Home Birth

Midwife Marsha Jackson reads Tonithia Reid’s records before giving the woman a prenatal exam at BirthCare & Women’s Health in Alexandria, Virginia. Wanting a home birth, Reid and her husband, Dominic Weeks, moved to Virginia near BirthCare about a month before Reid was due. Image by Karen Kasmauski. United States.

Tonithia Reid holds the hand of her husband, Dominic Weeks, as midwife Marsha Jackson draws blood during a prenatal appointment at BirthCare & Women’s Health in Alexandria, Virginia. Image by Karen Kasmauski. United States.

Best friend Page Johnson speaks to Tonithia Reid’s stomach during an Afrocentric blessing ceremony in Reid’s apartment in Alexandria, Virginia. Friends and family were invited to affirm their support of Reid and her baby during the ceremony. Image by Karen Kasmauski. United States.

As Tonithia Reid has a contraction on the couch, her husband, Dominic Weeks, tries to fill a birthing pool in the living room of their Alexandria, Virginia, apartment. Because none of the fittings for the hose matched the faucets in their apartment, Weeks ended up filling the pool one gallon at a time. A heating pad under the pool kept the water warm. Image by Karen Kasmauski. United States.

Doula Mayasa Telfair, center, updates midwife Marsha Jackson on Tonithia Reid’s labor. Only when Telfair was fairly sure Reid was ready to give birth did she call in Jackson. Reid delivered soon after the midwife arrived. Image by Karen Kasmauski. United States.

Doula Mayasa Telfair — who is also a certified midwife and former lawyer — manages Tonithia Reid’s labor as Reid sits inside a birthing pool in her Alexandria, Virginia, living room. Image by Karen Kasmauski. United States.

Midwife Marsha Jackson hands baby Zohra Marie Weeks to her mother following the delivery, which occurred about 30 minutes after Jackson arrived at the Alexandria, Virginia, apartment. Jackson believes the umbilical cord should remain attached until the baby cries out and shows it can breathe. Image by Karen Kasmauski. United States.

Dominic Weeks holds his newborn, Zohra Marie Weeks, following her birth in their Alexandria, Virginia, apartment, while his wife, Tonithia Reid, is attended to by the midwife. During the labor, Weeks was in the birthing pool with his wife. Image by Karen Kasmauski. United States.

As Tonithia Reid recovers from giving birth in her Alexandria, Virginia, apartment, midwife Marsha Jackson shows Dominic Weeks how to hold a measuring device to get his newborn’s official weight. Image by Karen Kasmauski. United States.

Midwife Marsha Jackson holds Zohra Marie Weeks after her delivery. Jackson stayed for hours after the birth to monitor mother Tonithia Reid and the baby and make sure they were healthy. Image by Karen Kasmauski. United States.

Midwife Marsha Jackson rolls her gear through an Alexandria, Virginia, parking garage. Jackson keeps the trunk of her car fully packed with the equipment and supplies she needs for the deliveries and postpartum visits she performs in Virginia, Maryland and Washington, D.C. Image by Karen Kasmauski. United States.

Tonithia Reid snuggles with her baby, Zohra Marie Weeks, during a postpartum visit from her midwife, Marsha Jackson. During the visit, Jackson checked the baby and mother and observed how well the breastfeeding process was going. An initial postpartum visit typically comes within 48 to 72 hours of the birth and can last several hours. Image by Karen Kasmauski. United States.
A New Focus

“We are facing a national shortage of obstetricians that is anticipated to get worse. We know that more outcomes in health care that tend to be the worst are in underserved, marginalized populations, and women often are in those particular populations. There’s a national crisis around maternal mortality, and a big part of that is the concepts of racism and cultural nuances that make it so that the people providing the care often are miscommunicating with the patient.
The need was there in the community and what we were able to do as a system is really delve into what innovation would look like and how to build a [midwifery] practice that’s sustainable for the future and that can also be replicated in our other facilities. We wanted to make sure that the people who were in the group were representative of the community and had a unique skill set in connecting with the community.”
— Amber Price, president of Sentara Williamsburg Regional Medical Center and certified midwife

During a prenatal examination, Nichole Wardlaw, a midwife working in Chesapeake, Virginia, speaks to the baby of her client, Earashea Bellamy, who is a week past her due date. Earashea and her husband, Freddie Bellamy, wanted their child to be delivered by a Black midwife. When they couldn’t find one available in their hometown of Richmond, they decided to use the services of Wardlaw, whose practice was close to where Earashea’s mother lives in Hampton, Virginia. The Bellamys stayed in Hampton during the last portion of her pregnancy. Though Wardlaw was able to deliver the baby at home, she took Earashea to Sentara CarePlex Hospital when the new mother started hemorrhaging. Image by Karen Kasmauski. United States.

Midwife Nichole Wardlaw visits Earashea Bellamy and newborn baby Amayah A’shea Bellamy at Sentara CarePlex Hospital in Hampton, Virginia. Because Wardlaw was working part-time with Sentara Midwifery Specialists at CarePlex, she was allowed hospital privileges when her client began hemorrhaging after giving birth. Earashea’s attending nurse, Sally Stokes, is pictured at right. Image by Karen Kasmauski. United States.

Midwife Nichole Wardlaw, right, speaks with a manager at Sentara CarePlex Hospital in Hampton, Virginia, after checking in with two clients who required a hospital stay. Having hospital privileges allows Wardlaw access to the technology of hospital care while also providing the personal experience of a midwife. Wardlaw’s practice also takes Medicaid and most insurances, making it accessible to many women and families; but not all midwifery companies take insurance or Medicaid. Image by Karen Kasmauski. United States.

Midwives Nichole Wardlaw, left, and Victoria Buchanan are pictured at Sentara Midwifery Specialists in Hampton, Virginia. Wardlaw, who had been up all night with a delivery and had another one scheduled for later that morning, naps as Buchanan finishes paperwork. Image by Karen Kasmauski. United States.

Midwife Victoria Buchanan sees patient LaChelle Evans at Sentara Midwifery Specialists in Hampton, Virginia. Both Evans and her husband, Darius Evans, are nurses and wanted a midwife delivery. They have two other children. Image by Karen Kasmauski. United States.

Midwife Victoria Buchanan, 28, follows up with patient Lexy Rogers, who had been induced a week early, at Sentara CarePlex Hospital in Hampton, Virginia. Buchanan had recently joined Sentara Midwifery Specialists at CarePlex, leaving a private practice to devote more time to midwifery and her clients. Image by Karen Kasmauski. United States.

Lexy Rogers takes a moment after the birth of her baby. Rogers had initially planned for a home birth for her fourth child but asked her midwife, Nichole Wardlaw, to induce her a week early, which meant she would deliver in the hospital. Image by Karen Kasmauski. United States.